For numerous trans women, male to female bottom surgery is not merely a medical procedure; there is significantly more personal importance involved than just operation. The surgery is often described as a vital personal transition: a movement towards aligning physically with who they truly are. The thoughts of undergoing bottom surgery can be thrilling, yet it comes with all the questions that arise with thinking about it. Experiences are generally based on anticipation of the appearance, created sensations, recovery processes involved, and expected long-term results.
At this moment, experienced surgeons have knowledge and capabilities to achieve surgical results that are not only aesthetically appealing but clinically satisfying. Very frequently, women will share that the experience of surgery was finally thinking, "I feel complete," and how it has contributed to their overall sense of well-being and fulfilled identity.
Understanding what constitutes "good results", the elements that become factors to being successful with surgery, and what the research indicates sexual satisfaction rates is necessary to help create more achievable situations, outcomes and experience for all who find themselves in this process of gender transition.
In this comprehensive guide, we'll be covering everything one needs to know about male to female bottom surgery results, from aesthetics and sensation to recovery and complications, including patient satisfaction. We'll also answer the most common FAQs, share real data, and discuss what "success" truly means beyond the operating table.
What is Male-to-Female Bottom Surgery?
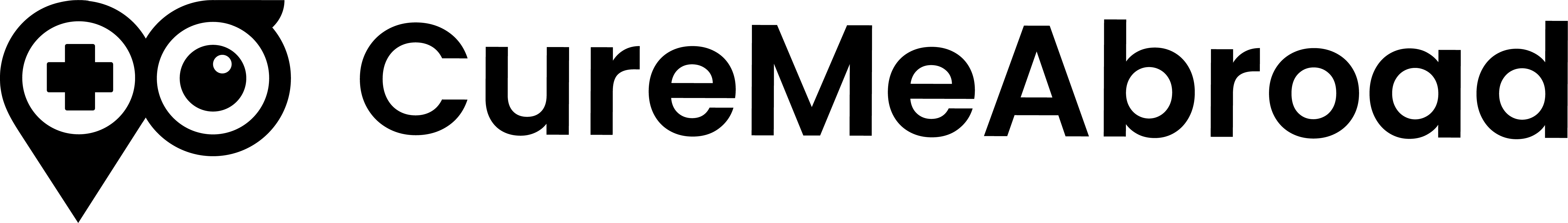
Broadly speaking, the bottom surgery for transgender women consists of creating a neovagina and an external female genital appearance from the natural male anatomy. Common techniques include:
- Penile‐skin inversion vaginoplasty (using penile and sometimes scrotal skin to line the neovagina)
- Peritoneal or intestinal (colon) vaginoplasty in selected cases, particularly where skin is limited
- Clitoroplasty (creation of a sensate clitoral structure)
- Labia creation (labia majora/minora)
- Urethral shortening and repositioning of the urinary meatus
Outcomes depend on the surgical technique, experience of the surgeon, preoperative conditions (hormone therapy, anatomy, health), and postoperative care.
Bottom Surgery MTF: Procedures
For some, having a male-to-female bottom surgery feels like a natural step. It's important to their sense of self. Others choose not to have it. People all relate to their bodies differently and should make individual choices that best suit their needs.
Now, take a look at the common MTF Bottom Surgery Procedures:
Vaginoplasty
This is the surgical creation of a vagina for transgender women. The penis, testicles and scrotum of the patient are removed and the skin is reused in the construction of a fully-sensitive and functioning vagina that includes a vaginal canal, labia and clitoris. In the technique called penile inversion vaginoplasty, the skin of the penis is inverted into a newly-created vaginal canal, preserving the nerves and sensitivity of the skin. Crane Center surgeons specialize in vaginoplasty and the penile inversion technique.
Orchiectomy
During an orchiectomy surgical procedure for transgender women, the testicles and scrotum are removed. Skin from the scrotum is used in the vaginoplasty procedure to create the labia majora as well as the vaginal vault. With the removal of the testicles, the vas deferens, the tubes that carry sperm, are cut and the patient will no longer be able to produce sperm or semen. Transgender women will be able to experience the feeling of orgasm, however. Talk to your doctor to learn more about what to expect after your orchiectomy and vaginoplasty surgery.
Vulvoplasty
Vulvoplasty is a procedure for transgender females in which the external genitalia are reconstructed as female, including labia minora and labia major, without the addition of the vaginal canal or vault. This is considered a gender-affirming surgery that is an alternative to vaginoplasty for transgender women who do not desire to engage in penetrative vaginal intercourse.
Also known as labiaplasty, this surgical operation utilizes the sensitive skin taken from the patient’s scrotum so that the newly created inner and outer labia have feeling. Creation of the clitoris, or clitoroplasty, is done using the highly sensitive skin from the glans of the patient’s penis.
Functionality and Sexuality after MTF Bottom Surgery
Vaginal depth/width and intercourse
Studies show that many patients were able to have regular sexual intercourse post‐surgery.
Some patients report neovaginal width sufficient for intercourse; others may have more limited width or require dilation frequently.
Sensation & orgasm
Sensation, especially erotic sensation, is one of the aspects that patients are least satisfied with. In one study, the least satisfaction in patients was with vaginal lubrication, vaginal touch sensation, and vaginal erotic sensation.
Clitoral sensation and overall genital sensitivity are enhanced with preservation of neurovascular bundles and proper surgical technique.
Urinary and other functions
Urination: Patients may note changes in the urinary stream, the direction of the stream, or the frequency. One series described urinary stream difficulties in about one‐third of patients.
Lubrication: Natural lubrication from neovagina is generally scant; most patients will have to use external lubrication for intercourse.
Dilation: The neovagina often requires lifelong dilation, especially in cases of sexual inactivity, to maintain depth/width and prevent stenosis. Following a dilation protocol is key to functional success in such cases.
Quality of life, psychology and gender identity: Many patients report improved quality of life, relief of gender dysphoria and enhanced sense of congruence with their gender identity. Higher satisfaction is related to functional sexual outcomes, good aesthetic male to female bottom results, and few complications.
MTF Bottom Surgery Cost
The cost for male-to-female bottom surgery varies greatly in different locations and with specific procedures, but it falls between about $10,000 and $30,000 in the US, whereas it costs much less in countries such as India and Thailand, at around $4,500 to $12,000. Elements that may change the final price include the surgeon's fee, the type of procedure-for example, vaginoplasty techniques such as scrotal skin grafting or peritoneal pull-through-and whether or not related surgeries such as orchiectomy are also included. Some US insurance plans also cover part of the expense.
Cost breakdown by location
- United States: The cost ranges between $10,000 and $30,000.
- Turkey: Costs are considerably much lower, lying between about $9,000 and $15,000 USD
- India: MTF bottom surgery in India ranges between about $4,500 and $12,000 USD.
- Thailand: Prices are more affordable, with procedures like scrotal skin grafting costing $4,500 and sigmoid colon vaginoplasty costing $10,000.
Male To Female Bottom Surgery Results: Healing and Recovery
Usually, healing from a male-to-female bottom surgery takes about 6 to 12 months, though the initial recovery takes more time. Salient features of the healed result include a neovagina that is functional and cosmetically satisfactory in appearance. Most patients are very satisfied with their results. Long-term outcomes rely heavily on diligent post-operative care, with consistent dilation critical to maintaining the neovagina depth and width over time.
Initial Recovery After Transfeminine Bottom Surgery
MTF bottom surgery could be a huge step for patients in their transformation journey. It is highly essential to be informed about post-operative recovery when one is deciding whether MTF bottom surgery is the right step for them.
Immediately after surgery, bottom surgery patients are observed for days by their surgeon. During this time, the medical staff aids in managing any post-op pain and monitors recovery to ensure everything goes smoothly.
Pain Management
Some discomfort is to be expected after surgery but can be managed with pain meds. There should not be significant pain. Follow all directions concerning medications to keep pain under control and to make recovery easier.
Wound Care
Wound care is usually done by your medical team in the immediate hours and days after surgery. They will check for infections, change the dressing and educate the patient on what to do when they return home. Good wound care is necessary to prevent complications and promote healthy healing.
Recovering at Home After MTF Bottom Surgery
The key in the first weeks of being at home is rest. No strenuous work or heavy lifting should be done; this can strain the surgical area. The patients are encouraged to take short walks to improve circulation, which helps in healing.
Dilation
One of the most important parts of MTF bottom surgery recovery includes dilation, which involves the use of medical-grade dilators to maintain the depth and width of the neovagina. Immediately after surgery, the neovagina will be packed with gauze, and a catheter will be in place; once this is removed, your medical practitioner will teach you how to dilate. Once instructed properly, patients can dilate on their own and are usually advised to do so many times a day during the initial months, reducing the frequency over time. Consistent dilation will prevent the neovagina from closing and allow for long-term functionality.
Hygiene
Good hygiene is important to prevent infection. The patients will follow their surgeon's recommendations regarding cleaning the surgical site and neovagina, usually by gently using non-irritating products and avoiding harsh or scented ones that might irritate the area.
Complications and Risk-Factors
No surgery comes without its risks. Below are some key complications and factors that need to be discussed as we talk about male-to-female bottom surgery results.
Common complications
- Stenosis/stricture of neovagina or neovaginal canal
- Fistula
- Tissue necrosis
- Prolapse of neovagina segments or upper/lower prolapse
- Urethral meatus stenosis
- Hematoma/excessive bleeding
- Urinary stream problems
- Granulation tissue formation
Male-to-female bottom surgery is a deeply profound and life-affirming procedure for many transgender women; it helps them bring their bodies into alignment with their true gender identity. With modern surgical techniques, most patients can realize high satisfaction rates, reporting significant improvement in body confidence, sexual function, and overall quality of life.
In the end, bottom surgery is not about anatomy; it's all about authenticity, comfort, and self-acceptance. For many, it marks the beginning of a new chapter, one where finally the reflection in the mirror feels like home.
Frequently Asked Questions
How long does it take to see "final" results?
Major surgery may take a few hours and the hospital stay is often days, but healing continues for months to a year or more. Swelling subsides, tissues settle, sensation may improve slowly. Many surgeons consider 12 months (or even 18 months) as the time when ‘results’ (appearance, depth, sensation) are stabilised.
What is the "regret" rate for MtF bottom surgery?
Data studies suggest that regret is very low at about 1% ranging from 0 to 3% in several studies. Regret does not equal dissatisfaction. Often, patients regret minor aspects or circumstances, not their decision to transition.
Does age or previous hormone therapy influence outcome?
Yes, younger and healthier patients have enhanced healing; longer hormone therapy prior to surgery might improve soft tissue conditions and prepare the patient better. However, age is not a barrier by itself provided health is good and counselling is adequate.
References
Feminizing Surgery - Mayo Clinic.
www.mayoclinic.org/tests-procedures/feminizing-surgery/about/pac-20385102American Society of Plastic Surgeons. “Transfeminine Bottom Surgery Results.”
www.plasticsurgery.org/reconstructive-procedures/transfeminine-bottom-surgery/resultsManrique OJ, Adabi K, Martinez-Jorge J, et al. Complications and Patient-Reported Outcomes in Male-to-Female Vaginoplasty Where We Are Today: A Systematic Review and Meta-Analysis. Ann Plast Surg. 2018 Jun;80(6):684-691. doi: 10.1097/SAP.0000000000001393. PMID: 29489533.
Hess J, Rossi Neto R, Panic L, Rübben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. Dtsch Arztebl Int. 2014 Nov 21;111(47):795-801. doi: 10.3238/arztebl.2014.0795. PMID: 25487762; PMCID: PMC4261554.