Let's face it: dealing with a chronic movement disorder like Parkinson's disease, Essential Tremor, or Dystonia can be incredibly frustrating. The tremors, the stiffness, the medication roller-coaster, it all chips away at your independence. If you've reached a point where medication isn't cutting it, or the side effects are just too much, you’ve likely heard about Deep Brain Stimulation (DBS).
It sounds a bit futuristic, but DBS is a thoroughly established, life-changing neurosurgical procedure. And if you're exploring it, you're not just looking for a fix; you're looking for your life back. This naturally leads to two huge questions: How does it work? And how much will this cost me?
We’re here to give you the honest breakdown, not just the technical jargon, but the straight talk on what DBS is, who it's for, and what your options are globally in 2025, specifically focusing on the competitive, high-quality markets of Turkey, India, Spain, and Israel.
What is DBS and How Does it Work? : The "Pacemaker for the Brain"
Consider your brain as a massive, intricate electrical network. In conditions like Parkinson's, specific circuits that make your movements smooth and coordinated start to misfire, sending out chaotic, irregular signals. This is what causes the tremors, rigidity, and slowness.
Deep Brain Stimulation (DBS) is essentially a targeted electrical tune-up for your brain.
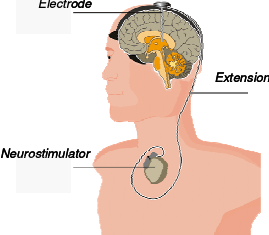
The Three-Part System:
The Lead (The Electrode): A very thin, insulated wire with multiple contact points (electrodes) on the tip. This is surgically implanted into a precise, tiny target area deep within the brain, such as the Subthalamic Nucleus (STN) or the Globus Pallidus Interna (GPi). The surgeon uses advanced imaging (MRI/CT) and sometimes real-time physiological mapping to ensure pinpoint accuracy.
The Extension Wire: This insulated wire is tunneled under the skin of your head, neck, and shoulder. Its only job is to connect the lead in your brain to the battery.
The Neurostimulator (The Pulse Generator/IPG): This is the battery-powered device, the "pacemaker" which is usually implanted just under the skin near your collarbone.
The Mechanism:
Once the system is in place and activated (usually a few weeks after the surgery), the neurostimulator sends continuous, mild electrical pulses through the extension wire to the electrodes in your brain.
Here’s the clever part: This continuous electrical current doesn't destroy brain tissue; instead, it blocks or disrupts the disorganized, faulty signals that are causing your symptoms. It's like inserting a noise-canceling signal into the chaotic electrical chatter. This results in a much smoother, more organized electrical rhythm, leading to a significant reduction in tremors, stiffness, and dyskinesias (medication-induced involuntary movements).
Am I a Good Candidate for DBS?
DBS is a powerful tool, but it’s not a magic cure, and it’s not for everyone. The best outcomes come from rigorous patient selection. You need to meet specific criteria, often determined through a multidisciplinary team evaluation (neurologist, neurosurgeon, neuropsychologist).
Who Generally Needs a DBS?
| Condition | Typical Candidate Profile | What DBS Helps Most With |
|---|---|---|
| Parkinson disease | You’ve had PD for at least 4 years. Your motor symptoms (tremor, rigidity, slowness) significantly improve when you take your main medication (e.g., Levodopa), but you suffer from "Wearing-off" (medication effects fading quickly) or Severe Dyskinesias (uncontrolled, wiggling movements caused by the medication). | Tremor, Stiffness, Slowness, Dyskinesia, Motor Fluctuations. |
| Essential tremor | Your tremor is disabling (interferes with eating, writing, etc.) and has failed to respond adequately to at least two different first-line tremor medications. | Tremor control (often 70-90% reduction). |
| Dystonia | Severe, generalized, or segmental dystonia that has been unresponsive to medication and significantly impacts quality of life. | Abnormal Postures and Muscle Spasms. |
Red Flags: When to Stop & Re-consider
- Poor Response to Levodopa: If your Parkinson’s symptoms don't improve noticeably after taking a high dose of Levodopa (the "challenge test"), DBS is unlikely to help.
- Severe Cognitive or Memory Issues (Dementia): DBS can sometimes worsen pre-existing severe cognitive issues. A thorough neuropsychological evaluation is mandatory.
- Atypical Parkinsonism: DBS is generally not effective for conditions like PSP, MSA, or Corticobasal Degeneration.
- Other Serious Medical Problems: Uncontrolled severe heart, lung, or psychiatric conditions that would make surgery too risky.
The takeaway: DBS should be considered when your medication is no longer providing consistent, high-quality, and on-time results, but still works when it's in your system. It's a tool to stabilize and extend those "good hours."
The Global Cost of DBS in 2025: A Medical Tourism Perspective
In the United States, a bilateral DBS procedure (electrodes in both sides of the brain) can easily range from $80,000 to well over $150,000 for the total package (hardware, surgery, hospital stay, and initial programming).
This is where medical tourism becomes an absolute game-changer. Our focus countries offer world-class, JCI-accredited hospitals and highly experienced neurosurgeons often trained in the West, but at a fraction of the price. The lower cost doesn't equate to lower quality; it reflects a lower cost of living, reduced overhead, and different insurance and litigation structures.
| Country | Estimated Total Package Cost (USD) | Key Advantage for Patients |
|---|---|---|
| Turkey | $20,000 – $35,000 | Best All-In Value. Highly competitive pricing often includes a more comprehensive package (flights, accommodation, transfers, translator). Excellent JCI-accredited hospitals, particularly in Istanbul, with high procedure volume. |
| India | $18,000 – $30,000 | Most Affordable. Very low pricing while maintaining high clinical standards and utilizing the same U.S./European-made devices. Strong reputation for medical expertise, especially in metro cities like New Delhi, Chennai, and Mumbai. |
| Spain | $45,000 – $60,000 | European Quality & Proximity. Higher cost than Turkey/India, but significantly lower than the U.S./UK. Excellent choice for European patients seeking a short flight, EU regulatory compliance, and high-end, modern facilities. |
| Israel | $55,000 – $75,000+ | Cutting-Edge Technology. High cost, similar to other major developed nations, but offers extremely advanced medical technology, leading research, and a very strong focus on precise neurological mapping and care. Price is often "on request" and variable. |
More Than Just the Surgery: The Full Journey
Choosing DBS is a process, not a one-off event. Your cost will cover two main stages:
Stage 1: The Implantation Surgery
Procedure: Placing the leads in the brain (often with the patient awake for optimal testing) and implanting the neurostimulator in the chest (usually under general anesthesia).
Inclusions: Hospital stay (typically 3-5 days), neurosurgeon and anesthesiologist fees, use of high-tech imaging equipment (MRI/CT), and the actual DBS device kit itself (the most expensive component).
Recovery: Initial recovery takes a few weeks. You'll need to avoid strenuous activity and not raise the arm on the side of the device above your shoulder for a month or so.
Stage 2: Programming and Optimization
Procedure: This is arguably the most critical part. A neurologist (a movement disorder specialist) uses an external programmer to communicate with the neurostimulator and carefully adjust the electrical settings (voltage, pulse width, frequency).
Timeline: This process is an art and a science. It begins a few weeks after the surgery, once the swelling has gone down, and typically takes 4 to 6 months of follow-up visits to find the absolute optimal settings that maximize symptom control while minimizing side effects. Your medication dosage will be gradually reduced during this time.
A note on packages: When reviewing costs, always ask your medical tourism provider exactly what is included. The lowest price might exclude the vital first year of programming adjustments or essential pre-operative diagnostics. Look for transparent, all-inclusive options.
Why the Price Difference Matters
The cost savings aren't just about a better vacation fund; they’re about access to care. For many, the difference between a $120,000 procedure and a $25,000 procedure is the difference between regaining control of their life and simply learning to live with their disability.
Choosing a destination like Turkey or India allows you to tap into experienced, high-volume centers that specialize in DBS, ensuring you get a dedicated team. Choosing Spain or Israel offers a different blend of geographic convenience and advanced medical infrastructure.
Deep Brain Stimulation: 5 Essential FAQs
1. Is DBS a cure for Parkinson's Disease or Essential Tremor?
No, DBS is a treatment, not a cure. DBS effectively manages and significantly reduces the severe motor symptoms (tremor, stiffness, slowness, dyskinesia) by modulating abnormal brain signals. It provides years of improved quality of life and function. However, it does not stop the underlying neurological disease (like Parkinson's) from progressing. Think of it as hitting the 'reset' button on your movement quality for a long time, but the battery in the brain's engine still needs to be monitored.
2. Will I still need to take my medication after DBS surgery?
Most likely, yes, but often much less. The goal of DBS, especially for Parkinson's, is to reduce the dosage of medications like Levodopa, which in turn minimizes the medication side effects, such as disabling dyskinesias. The majority of patients find a balanced regimen where they rely less on pills and more on the stimulation. For Essential Tremor, the dependence on medication is often eliminated or drastically reduced.
3. How long does the battery/device last, and what happens when it runs out?
It depends on the device type:
- Non-Rechargeable Systems: Last approximately 3 to 5 years.
- Rechargeable Systems: Can last up to 15 to 25 years with regular charging.
When the battery runs low, you will undergo a quick, minor outpatient procedure (called a generator replacement) to swap the old pulse generator in your chest with a new one. The wires in your brain stay exactly where they are. This follow-up surgery is simple, low-risk, and much less complex than the original implantation.
4. When will I start seeing the benefits after the surgery?
You'll see initial healing within weeks, but the real benefits are a gradual process over months. The surgery itself is only Step 1. Your device will be activated a few weeks later, once swelling has subsided. The true improvement comes during the programming and optimization phase, where your neurologist fine-tunes the electrical settings over 4 to 6 months. Be patient, it takes time for the team to find the "sweet spot" that gives you the best results.
5. What are the main risks of the surgery I should be aware of?
DBS is a low-risk procedure in experienced hands, but the most serious risks are related to the brain procedure itself. The two primary surgical risks are a small chance of bleeding in the brain (intracranial hemorrhage) or infection at the surgical site.
Modern stereotactic techniques keep the risk of bleeding very low (typically less than 1-3%). Other rare risks include lead (wire) misplacement or temporary side effects from the stimulation (like speech changes or tingling), which are usually correctable by adjusting the programming.